Keratoconus
Definition of Keratoconus
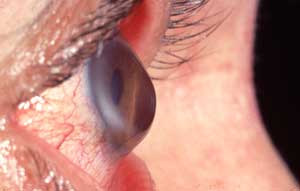
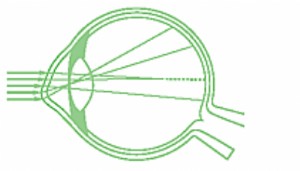
Keratoconus is a conical dystrophy of the cornea of unknown origin, charactarized by a protrusion of the lower part of the cornea. It is not bound to any inflammatory process and shows up during the adolescence. The sharpness of vision is reduced due to a progressive irregular deformation of the cornea (irregular astigmatism) and in extreme circumstances to scarring of the cornea. In general keratoconus affects both eyes but can also develop asymmetrically. The vision is affected from the moment that the irregularity of the cornea can no longer be corrected by means of glasses or contact lenses or induces visual instability.
Treatments
Intrastromal corneal ring segments
Ultra Violet Crosslinking
Surgical visual rehabilitation after UV-CXL
High-Intensity UV Crosslinking
If you want more information, or would like to make an appointment:
Contact us or call 0032 (0)2 741 69 99
Frequency
Keratoconus can occur in several circumstances: as an isolated process, combined with another ocular disease or associated with a general condition.
The frequency of keratoconus is still uncertain: extended studies have shown that it affects 50 to 230 persons on 100.000.
Keratoconus usually starts during puberty and develops over a period of 10 to 20 years, in 82% of the cases before the age of 40. It is still uncertain whether women are more affected than men. Probably there is no geographical, cultural of social predisposition.
Causes
The causes of this condition remain mysterious. The role of heredity is brought forward during observation of much familial cases. 7% of the patients should have at least one other family member that suffers from keratoconus. At least 10% of the descendants have the risk to develop keratoconus if one of the parents is carrier of keratoconus.
This deformation of the cornea can go together with other disorders like trisomy 21 or other deviations that affect conjunctival tissues (disease of Ehler-Danlos). There should also exist an association with multiple rubbing in the eyes during the youth.
It also occurs with persons who have a history of atopia (asthma, eczema).
Symptoms
Keratoconus is generally recognised with an adolescent or a young adult, between the age of 10 to 20 years that come on a check up because of a disturbed vision and a visual deformation. This can go together with photophobia (increased light sensitivity) and light dispersal. In an advanced stage the vision can diminish quickly because of fog. The cornea becomes untransparent because of the process of scarring in the cornea. These symptoms occur mainly with myopia. Sometimes the patient complains about pulsative vision, mainly after a physical effort and this shows in the becoming thinner of the cornea.

Diagnosis
The clinical examination goes together with the proof of the 3 caracterial changes of the disorder:
The irregular astigmatism can be shown in different ways:
- Retinoscopy
- Keratometry (measurement of the curvatures of the cornea) is very important. In the beginning, irregular astigmatism is the only element that can show keratoconus.
- Topography of the cornea (using a Placido disk) is an exam that allows to make a map of the cornea with the measuring of the curvatures of the different areas of the cornea, like the examination of the irregulatities of a mountain. This exam shows graphical results that are very clear and that can be compared to document the possible progression of the keratoconus.
The unusual protrusion of the cornea can be determined with a splitt lamp exam. In a further stadium the cornea becomes thinner with the occurrence of untransparent cicatrices.
Evolution
Keratoconus does not necessary cause blindness but the myopia and astigmatism increase and the astigmatism becomes more and more irregular. This explains why the vision suffers from an always larger deformation. The problem is progressive, needs years to develop completely but can stabilise in each stadium. The progression of the disorder occurs mainly between the age of 10 and 20 years: she will become slower between the age of 20 and 30 and is very limited after 30 years.
In rare cases the disorder evolves to Acute Keratoconus. The cornea becomes so thin that can cause a rupture of the endothelium (inner membrane of the cornea) with oedema of the surrounding tissues.
Treatment
The treatment of the keratoconus depends on the seriousness of the disorder.
Initially glasses can correct the astigmatism with certain success. These glasses can seldom be endured constantly and the patients are often disappointed about the bad quality of the vision. It has to be insisted with the patients to endure the correction with glasses as long as possible to slow down the anatomic aggression caused by the wearing of contact lenses.
When the periphery of the cornea is affected by the cone (keratoconus), the irregular astigmatic deformations of the cornea can only be corrected best by means of hard contact lenses. There exist today more and more possibilities to adjustment of contact lenses for keratoconus.
Eventually, when the vision can no longer be corrected optimally with contact lenses or if the patient develops an intolerance to contact lenses, a corneal transplant is recommended (penetrating keratoplasthy PKP). This is only necessary in 10% of the cases. The central part of the damaged cornea is removed and replaced by a graft of a deceased person. Keratoconus represents 8 to 12% of the indications for corneal transplants. The visual results that are achieved are reasonable: post-operatifvely unpredictable astigmatism is often present that can be treated in a second stage – not earlier than one year after the keratoplasty, after the removal of the stitches – with excimer laser techniques (topography-guided PRK or LASIK).
Since a few years there is the possibility to stabilise the irregular deformation of the cornea by means of Ultra-Violet Crosslinking. After impregnation of Vitamine B2 (Riboflavine), the cornea is exposed to ultra-violet radiation: the structure of the Riboflavine changes what results in a reinforcing effect on the cornea. Once the stability of the cornea has been determined, the irregular astigmatism can be caught in a second step by surface excimer laser techniques: topography-guided PRK.
If you want more information, or would like to make an appointment:
Contact us or call 0032 (0)2 741 69 99