Strabismus
What is strabismus?
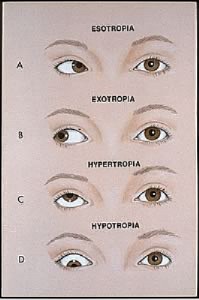
Strabismus is a visual disorder where the eyes are misaligned and point in different directions. This misalignment can occur part of the time (intermittent) or all of the time (constant). Strabismus is classified according to the direction of misalignment. When one eye is looking straight ahead, the other eye may turn inward (esotropia or convergent), outward toward the ear (exotropia or divergent), downward (hypotropia) or upward (hypertropia).
Strabismus occurs in approximately 2% of children under 3 years of age and about 3% of children and young adults, affecting boys and girls equally. Normal alignment of both eyes during childhood allows the brain to fuse the two pictures into a single 3-dimensional image. This allows a high degree of depth perception. In children, when the two eyes fail to focus on the same image, the brain may learn to recognize the stronger image and ignore the weaker image of the amblyopic eye, to avoid double vision. If this is allowed to continue, the eye that the brain ignores will never see well. This loss of vision is called amblyopia. Amblyopia results if vision from one eye is consistently suppressed and the other eye becomes dominant. Among children with strabismus, one-third to one-half develop amblyopia.
If strabismus develops for the first time in adulthood, the affected individual usually experiences double vision. Because the brains of adults are already developed for vision, the problems associated with amblyopia, in which the brain ignores input from one eye, do not occur with adult strabismus.
What causes strabismus?
The exact cause of the eye misalignment that leads to strabismus is not fully understood. However, strabismus is certainly more common in families with a history of the disorder.
Six eye muscles control eye movement an are attached to the outside of each eye. To focus both eyes on a single target, all eye muscles must work together with the corresponding muscles of the opposite eye. The brain coordinates these eye muscles. It is important to understand that it is usually not just one eye that is deviated, but rather, the eyes are misaligned in relation to one another. In essence, both eyes are usually at fault, although one eye may appear to be the “crooked’ one.
Acquired strabismus in adults can be caused by injuries to the orbit of the eye or brain, including closed head injuries and strokes. People with diabetes often have loss of circulation causing an acquired paralytic strabismus. Loss of vision in one eye from any cause will usually cause the eye to gradually turn outward (exotropia).
Strabismus can be caused by problems with the eye muscles, with the nerves that control the eye muscles or with the brain, where the signals for vision are processed. Strabismus can accompany some illnesses such as high blood pressure, multiple sclerosis, myasthenia gravis, or thyroid disorders.
Signs and symptoms
Newborns often appear to have crossed eyes due to a lack of developed vision, but this disappears as the infant grows. True strabismus does not disappear as the child grows.
Strabismus can often be recognized by a casual observer. In fact, most cases of strabismus are first noted by a parent or the child’s pediatrician prior to examination by an ophthalmologist. Children should be monitored closely during infancy and the preschool years to detect potential eye problems, particularly if a relative has strabismus.
Symptoms of strabismus include:
- Eyes that look misaligned.
- Eyes that did not appear to move together
- Frequent blinking or squinting, especially in bright sunlight
- Tilting the head to look at things
- Faulty depth perception
- Double vision
Diagnosis
The doctor will evaluate the alignment of your child’s eyes, looking for evidence of uncoordinated eye movements. In infants and young children with limited ability to cooperate, the doctor will test alignment by comparing the position of a light reflecting off each eye. However, this test may not detect intermittent strabismus unless the strabismus is occurring at the time of testing. In children who are able to cooperate, both intermittent and constant strabismus can be detected using the “cover-uncover” and “alternating cover” tests. In these tests, the child stares at an object and the examiner watches the response of each of the child’s eyes when the other is covered and uncovered.
Some ophthalmologist screen for vision problems with a special camera that takes instant pictures of a child’s eyes.
The patient may be asked to look through a series of prisms to determine the extent of eye divergence. The eye muscles will be tested to determine the strength of the extraocular muscles.
A comprehensive eye exam, including a retinal evaluation, is needed to rule out pathological causes for the eye turn. A measurement also is taken to obtain the best vision correction with glasses. Additional testing may be needed depending on the cause of the eye turn.
Children should be monitored closely during infancy and the preschool year to detect potential eye problems. The earlier the diagnosis and treatment, the better the visual results.
Treatment
The treatment goal for strabismus is to preserve vision, to straighten the eyes, and to restore 3-dimensional vision. Treatments vary, depending on the type and cause of strabismus. If your child’s strabismus has caused amblyopia, treatment will aim at bringing the vision up to normal in the “lazy” eye first.
- Glasses may help straighten the eyes.
- A patch can be worn over the preferred eye to force the child to use the weaker or suppressed eye.
- Eye drops are used to temporarily blur the vision of the preferred eye for the same purpose. Exercises may be prescribed to strengthen specific eye muscles.
Forcing a child to use the weaker eye can improve sight by reinforcing the connection between the eye and the brain.
Surgery on the eye muscles may be necessary, especially when glasses are not enough to straighten the eyes. It’s important to understand that strabismus surgery does not resolve amblyopia. However, the majority of children with strabismus will eventually require strabismus surgery to better align the eyes. This shot operation typically is done under general anesthesia and may involve one or both eyes. Strabismus surgery commonly entails recessions of eye muscles if weakening of muscles is required, and resections of eye muscles when strengthening of eye muscles is required.
Recovery time is rapid and the patient is usually able to resume their normal activities within a few days. Over-or-under correction can occur and further surgery may be needed. As with any surgery, eye muscle surgery has certain risks which include infection, bleeding, excessive scarring, and other complications that can lead to loss of vision.
In some cases, surgery can be avoided by using a relatively new technique in which a drug botilinum) is injected into one or more eye muscles to temporarily paralyze the muscle. While one muscle is relaxed, the opposing muscle can tighten, shifting the alignment of the eye. Although the effect of the medication eventually wears off, the opposing muscle that has tightened remains that way, often making the correction permanent.
If you want more information, or would like to make an appointment:
Contact us or call 0032 (0)2 741 69 99